Katie did not have a doula at her first birth and decided to get some extra support the second time around in hopes that she could reach all of her birth goals and she did! Everything went exactly as she'd planned it and it was really great to see how well her birth plan was respected by her providers.
Started having contractions for two weeks prior to delivery. The week prior to delivery I had a membrane sweep and was at 2 cm. Contractions picked up but didn’t lead anywhere the rest of the week.
The following week I went in for my midwife appointment after having nonstop mild contractions for 24 hours to learn I was at 4 cm with a bulging water bag. We did another membrane sweep during this exam and baby was at a -2 station as well.
After that appointment ended at 11 am, the contractions just increased in intensity and got closer together as well. At this point I sent Suzanne, my doula, a screen shot of my contractions for the past 50 minutes and they where about 4-8 minutes apart. She suggested eating some lunch and once we see all 5 minute contractions, head on in to the hospital. Well, this happened pretty quickly. I walked around the house and did some laundry and dishes to keep busy while going through each wave and knowing they were for sure getting stronger. My husband came home from work just as I was ready to walk out door.
 Katie enters transition
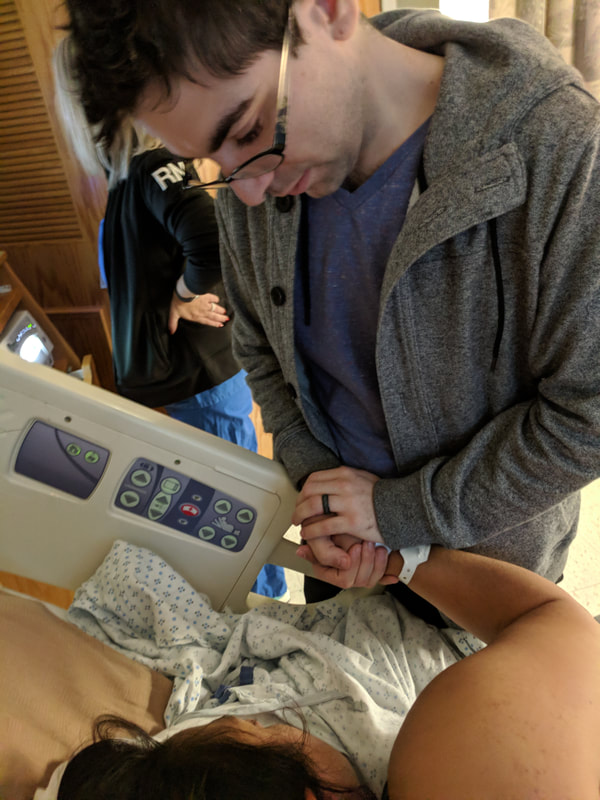
Katie enters transition We were at triage by 2:30 and was already to 6 cm and contracting every 90 seconds. Once I was admitted to a room I got to go over my birth plan with the midwife on call. Thanks to Suzanne’s help, I was able to write up a plan that was reasonable and what I wanted and to my utmost shock I got to have the labor I wanted to the T. Nothing varied. It was so nice to have my mom and husband be able to be here as support along with Suzanne who helped guide me through the labor. I had requested to use the nitrous-gas machine while laboring and it was available!
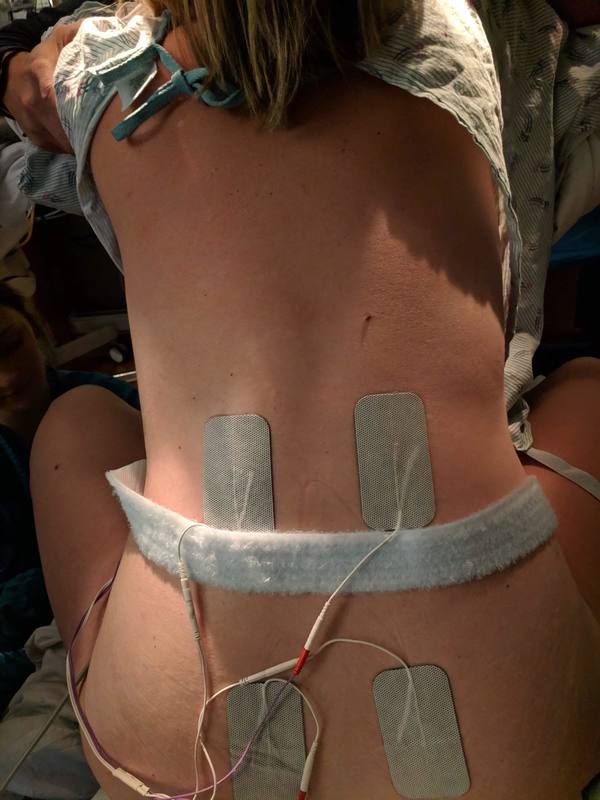
Suzanne had joined us at about this time and I was still breathing and moving around the room through contractions. I used the nitrous for maybe an hour or so off and on, but was I coming to transition I found it made me more nauseous then helpful. During these contractions Suzanne helped with counter pressure and encouraging words. Once I was tired and ready to lay down for a bit she continued to remind me to breathe deep and slow, tell me I am do this, I am having a baby. All very reassuring things I needed to hear. As things came on very strong I noticed the baby warmer and more nurses were coming in the room.
I remember us talking about how these are all signs baby is about to be here and I’m getting to the finish line. So that was a another wonderful thing to know with being told in the moment and that really helped me stay focused. At this point the midwife asked if I wanted to have my water broken because it was bulging and probably the last thing to keep me from pushing this baby out. As I said yes, I felt a strong push sensation and Suzanne and the nurse encouraged me to push hard, as I was about break my water on my own. It was such a cool experience to feel it burst. To also hear the support from Suzanne and the nurses that I did it was great and so reassuring.
 I help baby Thomas latch after birth
I help baby Thomas latch after birth 






















 RSS Feed
RSS Feed