I was with Katie for her first birth in 2015 and was so excited to hear she was pregnant again. The biggest compliment a client can give me is to hire me again! Here is the birth story of her second baby, Eliza, in her own words.
~Suzanne
 Katie's husband Phil helps her balance on a yoga ball as she leans into an inversion to help reposition her crooked baby. Labor picked up after we helped baby get straightened out.
Katie's husband Phil helps her balance on a yoga ball as she leans into an inversion to help reposition her crooked baby. Labor picked up after we helped baby get straightened out. Preface: I had wanted a drug free labor with my first baby, Ethan, but after two nights of no sleep from early start and stop labor (and hearing the agony of the woman in the room next to mine going through drug free transition and delivery), I decided to have an epidural so I could rest before pushing. It was a great experience and the only negative side effect was a lazy bladder afterwards ... I ended up going home with a catheter for 24 hours. This time I was open to an epidural but did hope to have a shorter labor and enough energy to avoid one. I had also learned the hospital I would deliver at recently acquired a nitrous oxide machine and I was eager to try that as a coping technique.
Eliza's birth: I have some bloody show Sunday morning. I experience 90 minutes of mild contractions from 4-5:30 am on Monday and have a bit more bloody show and some looser stools. I take an hour long morning walk with Ethan to hopefully get things going and have mild contractions here and there throughout the day and a scant amount of bloody show. I go to bed at 8:30 pm, anticipating contractions to start up. I wake from a stronger contraction at 10:30 and again at 11:30 and 12:30. I can no longer sleep through them at this point. They seem to be 5-7 min apart and lasting about 45 seconds. This continues for the next several hours. I am able to cope with deep breaths and slow exhales until they pick up in intensity at about 3:30 am and I start vocalizing a bit to get through them. At 5 am I stop trying to sleep between them and get up to eat some breakfast and see if being more active gets them coming closer together. They’re about 4-5 minutes apart when I do this. My husband Phil starts pushing on my back as I lean over the counter and this helps me cope along with vocalizing. We decide to load the car for the hospital around 5:30. The contractions slow down a bit but pick back up close to 7 am. I call Triage to let them know we’re about to head in. They advise me to labor at home a bit longer and we consider staying until Ethan wakes up so we can remind him where we are going and why, but our doula Suzanne lets us know contractions will probably slow down for a while when he’s around. So we leave for the hospital at 7. I have three contractions in the car during the 15 minute ride and then another 3 closer together walking from the car in to Triage. Of course, once I get checked in to Triage and set up on the monitor, things slow way down again. But my cervix is checked and I’m 4.5cm dilated. They decide to admit me. I let them know right away that I would like the nitrous oxide machine as soon as it becomes available. Contractions continue about 7 minutes apart when I first get to our room and they place an IV lock. By 8:30, our doula Suzanne has arrived and the admission process is complete. The doctor does an ultrasound to check baby’s position and we discover the head is down but off to the right and will need some repositioning. I eat some breakfast and then we start walking the halls to get the contractions to pick up again. Over the course of the next couple hours, we alternate walking and returning to the room for intermittent monitoring of baby’s heartbeat. I am able to cope with vocalization and Phil and Suzanne doing counter pressure on my back. Around 10:30, Suzanne has me do an inversion exercise and some squat leans to reposition baby. Contractions range from 4-7 minutes apart. I also spend some time sitting on the toilet and this helps progress the effacement.
Eliza's birth: I have some bloody show Sunday morning. I experience 90 minutes of mild contractions from 4-5:30 am on Monday and have a bit more bloody show and some looser stools. I take an hour long morning walk with Ethan to hopefully get things going and have mild contractions here and there throughout the day and a scant amount of bloody show. I go to bed at 8:30 pm, anticipating contractions to start up. I wake from a stronger contraction at 10:30 and again at 11:30 and 12:30. I can no longer sleep through them at this point. They seem to be 5-7 min apart and lasting about 45 seconds. This continues for the next several hours. I am able to cope with deep breaths and slow exhales until they pick up in intensity at about 3:30 am and I start vocalizing a bit to get through them. At 5 am I stop trying to sleep between them and get up to eat some breakfast and see if being more active gets them coming closer together. They’re about 4-5 minutes apart when I do this. My husband Phil starts pushing on my back as I lean over the counter and this helps me cope along with vocalizing. We decide to load the car for the hospital around 5:30. The contractions slow down a bit but pick back up close to 7 am. I call Triage to let them know we’re about to head in. They advise me to labor at home a bit longer and we consider staying until Ethan wakes up so we can remind him where we are going and why, but our doula Suzanne lets us know contractions will probably slow down for a while when he’s around. So we leave for the hospital at 7. I have three contractions in the car during the 15 minute ride and then another 3 closer together walking from the car in to Triage. Of course, once I get checked in to Triage and set up on the monitor, things slow way down again. But my cervix is checked and I’m 4.5cm dilated. They decide to admit me. I let them know right away that I would like the nitrous oxide machine as soon as it becomes available. Contractions continue about 7 minutes apart when I first get to our room and they place an IV lock. By 8:30, our doula Suzanne has arrived and the admission process is complete. The doctor does an ultrasound to check baby’s position and we discover the head is down but off to the right and will need some repositioning. I eat some breakfast and then we start walking the halls to get the contractions to pick up again. Over the course of the next couple hours, we alternate walking and returning to the room for intermittent monitoring of baby’s heartbeat. I am able to cope with vocalization and Phil and Suzanne doing counter pressure on my back. Around 10:30, Suzanne has me do an inversion exercise and some squat leans to reposition baby. Contractions range from 4-7 minutes apart. I also spend some time sitting on the toilet and this helps progress the effacement.
 Katie's hospital has only one nitrous oxide machine ... so she had to wait until other patients were done with it before it could be brought to her.
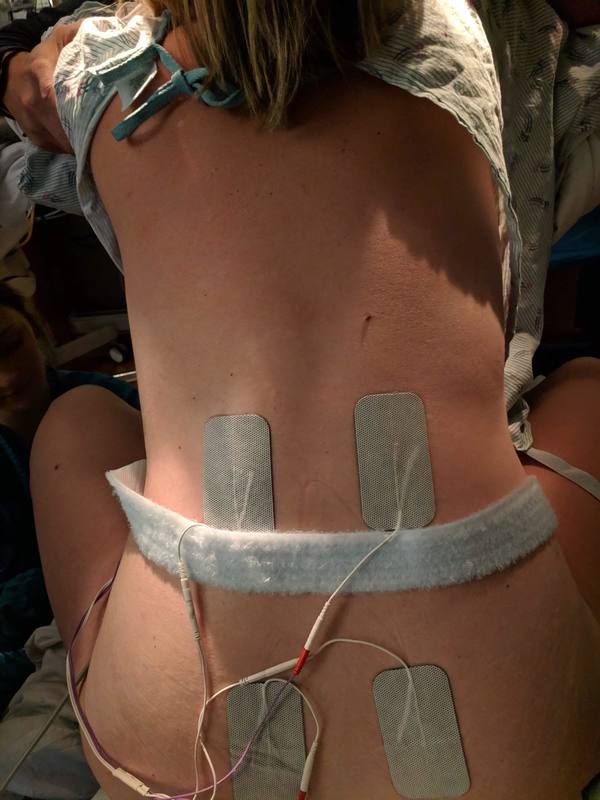
Katie's hospital has only one nitrous oxide machine ... so she had to wait until other patients were done with it before it could be brought to her. Around 12, Suzanne sets me up with the tens unit and I start to use that along with vocalization to cope. We alternate walking in the hall, leaning on the bed/ball, and sitting on the toilet. I like sitting on the toilet, but my legs keep falling asleep, so we try putting my feet up on stools which puts me in a squatting position. This continues to help effacement and I have more and more bloody show. My cervix is checked and I’m about 6-7 cm. I continue hall walking, sitting on the toilet, and leaning against the ball on the bed. At this point, the contractions are getting longer and intense and I’m really feeling the need for a rest. I have an emotional moment from exhaustion. I’m sure both Phil and Suzanne think I’m on the verge of asking for an epidural, but I don’t. We inquire again about the availability of the nitrous oxide and it’s rolled into my room shortly thereafter, around 2pm. Perfect timing as I am really needing that rest and the nitrous allows me to lie in bed and relax enough to cope with the contractions lying down, with a peanut ball between my legs to continue encouraging the baby to come down. The gas doesn’t take the pain away but gives me something to focus on and makes me feel less anxious as I come out of a contraction. The nitrous reaches to the toilet as well so I sit there for a while. Then I get on all fours on the bed and rest on the ball. I’m getting emotional from the pain and Suzanne encourages me to vocalize more aggressively. This goes on for several contractions and then Suzanne tells me to look behind me. I see the nurses setting up the baby station and she tells me they believe in me. It’s at this point I realize how far I have come and that I can do this. I get very emotional but knowing the end is in sight is encouraging. The doctor checks my cervix again around 4pm and I’m basically complete except for a little lip. We decide it’s time to break my water and baby is low enough that it’s safe to do so. Afterwards, they let me labor down a bit and then tell me I can start pushing. It’s about 4:50pm. The contractions are extremely intense at this point and fairly close together. I’m vocalizing very loudly and have the tens unit cranked up to high. I’m still using the nitrous but it’s not as helpful. I push for several contractions in a row, but I’m checked again and baby isn’t really moving down. We decide to let gravity help and the nurses attach the squat bar to the bed. I realize that the nitrous isn’t helping at this point and I need two hands for the squat bar (the nitrous mask can only be held by me) and to put all my energy and focus on pushing. I push for a couple contractions in the squat position. The contractions seem close together to me and I’m in such pain that it’s difficult to differentiate between contractions and rest periods. I get very emotional again and say I just need to rest. I just want it to be over and know the only way for it to be is to push hard. I push with all my might and can feel the head crowning. Realizing I’m so close, I just push as hard as I can. The attending doctor recognizes the risk of bad tearing and tells me to lie back so she can help minimize the damage. Phil kisses me and I can see how proud he is of me and how close we are to meeting our baby. A few more pushes and the team all gets very excited and tells me baby is about to come out. Another push and she’s out at 5:29pm. Instant pain relief and euphoria! They put her on my chest and I see she’s a girl before Phil even has a chance to announce it out loud. He excitedly announces what he knew all along and I’m shocked and so happy. She is crying and perfect in every way. Phil tells me to announce her name and I say Eliza immediately. No question. After a few minutes and a shot of pitocin, I deliver the placenta with another gentle push. Then the damage is assessed by the attending and resident. A bucket handle tear and a couple other tears require stitches. I’m given a shot of lidocaine but the 30 minute repair and subsequent belly massages are still incredibly painful. I just try to focus on my baby girl and once they are done I am able to relax enough to breastfeed. She latches fairly easily and nurses like a pro. I’m so happy and express my gratitude to my amazing birth team. I was so lucky to labor and deliver all within one shift and had the same awesome nurses and doctor from beginning to end. What an incredible experience. I am so very blessed. And still surprised that I ended up doing it without drugs/epidural! Hardest thing I have ever done in my life, marathon included.
Side note: Ironically, even without the epidural, I am unable to pee for several hours afterwards. The postpartum nurse makes me some special tea combination, encourages me to walk around, and threatens a bladder scan and catheter if I’m unable to pee by 10 pm. Luckily, the tea does the trick! I am now one week postpartum and haven’t experienced any complications, just the normal swelling.
Side note: Ironically, even without the epidural, I am unable to pee for several hours afterwards. The postpartum nurse makes me some special tea combination, encourages me to walk around, and threatens a bladder scan and catheter if I’m unable to pee by 10 pm. Luckily, the tea does the trick! I am now one week postpartum and haven’t experienced any complications, just the normal swelling.


 RSS Feed
RSS Feed