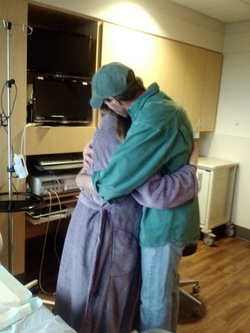
 Kyle and I help Rachel through a contraction.
Kyle and I help Rachel through a contraction. However, this fear is incredibly unfounded. It is true that occasionally dads are fearful of the process and need a lot of space and breaks, making the hiring of a doula essential to ensure the mother receives the support she needs. But in most cases, the dad wants to help and wants to be involved, but just isn't sure what to do or how to do it.
As a trained birth professional, it is my job to know when the mom needs to hear specific encouragement, such as, "Yes, this is absolutely normal. Your body is shaking due to the hormones of labor, it's from working very hard and it happens to nearly everyone. Nothing is wrong, no you aren't going into shock" and when she just needs strength and love. The former is best provided by me, and the latter is absolutely best provided by her partner. My favorite moment in a birth when the dad steps up and tells the mama how absolutely beautiful and strong she is and how much he loves her.
At that point, I might also be involved, providing physical support like massage or counter-pressure, but sometimes I just step back to give them space. If the dad is looking to comfort her physically, I can take a quick moment to show him where and how his strength might be best applied, but often it's not worth interrupting their connection.
I find that birth is an ebb and flow of energy and this is absolutely true for the partner and doula as well. One of the very best aspects about having a doula at your birth is the ability to trade off with support roles so that eating, using the restroom and power-napping can take place as needed without abandoning the birthing mama. I have supported a few military families during deployment and let me tell you, I do this for a living and those births left me completely exhausted. A father providing sole support for his partner while he himself has so many emotions to process at the same time sounds very challenging.
A metaphor that often speaks to guys is that if your team was going to the superbowl, but had never even played football before, would you also bring a coach who had never coached before? Or would you try to find someone with a lot of knowledge to help you learn what you needed to know?
Giving birth is the hardest work a woman will ever do and it is my job to help make sure that both partners are emotionally present and grounded when they welcome their babies into the world. Sometimes I take a lead role, and sometimes I step back and just bask in the amazing process that is birth.






















 RSS Feed
RSS Feed